Several weeks ago I summarized the evidence that demonstrates that when you delay cancer chemotherapy and substitute alternative medicine, you die sooner. Thank you to the tireless Edzard Ernst, who identified non-cancer evidence that demonstrates how choosing complementary and alternative medicine (CAM) instead of real medicine, can cause harm. In this case, the example is early inflammatory arthritis (EIA), and what was studied was the relationship between CAM use, and the delay to initiation of medical therapy. Time is of the essence with inflammatory arthritis, as there are medications that can reduce the risk of permanent joint damage. This new paper adds to the accumulated evidence to show that CAM, while it is commonly thought to be harmless, can indeed harm – not only from direct effects, but also from delaying the initiation of proper, effective medical treatment.
What is inflammatory arthritis?
Inflammatory arthritis is a term that describes inflammation of the joints (and other tissues). Inflammatory arthritis can include rheumatoid arthritis, and several other conditions. These are often autoimmune conditions, where your immune system treats its own tissues as foreign, and attacks it. Pain, swelling and tenderness are typical with inflammatory arthritis, and a diagnosis is usually based on a physical examination and laboratory tests. There are now many medications that can treat arthritis, ranging from the non-steroidal anti-inflammatory drugs (NSAIDs) such as naproxen and ibuprofen, to disease-modifying anti-rheumatic drugs which include biologic drugs that can be very effective and even put the disease into remission. While inflammation can be treated, joint destruction from arthritis can be permanent, so starting appropriate therapy, quickly, is important to reduce the risk of long-term damage. Today, aggressive treatment early in the course of the disease is considered to be the standard of care, so it is important for new cases to be recognized and referred for specialist assessment as quickly as possible. Barriers to early treatment include patient delays, but also system delays like wait times for referrals. Understanding why patients may not seek treatment is a question that led to this most recent study.
Studying CAM and inflammatory arthritis
Complementary and alternative medicine (CAM) is commonly used in different cultures, including Asian cultures, where traditional Chinese medicine may even be government-endorsed, despite the lack of evidence to show it is an effective system of medicine. When a group of researchers identified that many patients with a new diagnosis of arthritis had tried CAM prior to seeking medical treatment, they hypothesized that CAM may be delaying referral and medical therapy.
This paper is from Manjari Lahiri and colleagues and was published in the International Journal of Rheumatic Diseases. Entitled “Use of complementary and alternative medicines is associated with delay to initiation of disease-modifying anti-rheumatic drug therapy in early inflammatory arthritis”, this was a prospective survey of patients with EIA. All patients seen at one of two hospitals in Singapore where they were invited to participate. Patients were included if they had a self-reported symptom of EIA, which was defined as inflammation of two or more joints, not caused by trauma. Patients were assessed at 3, 6, and 12 months, then annually for 3 years. All participants completed a nurse-administered questionnaire on demographic, health and lifestyle factors including CAM use. In this study, CAM was defined as the ingestion of tablets, herbs, powders or drinks purported to have medicinal properties. They could be prescribed (e.g., by a practitioner in traditional Chinese medicine) or purchase over the counter. Acupuncture, therapeutic massage and cupping, when used for the purpose of a therapeutic effect where included in the definition of CAM, while exercise (including yoga and tai chi), physiotherapy, and occupational therapy were not considered CAM. (This is among the more accurate delineations of CAM/non-CAM I’ve seen in a study.)
CAM users delay treatment
For this study, only the baseline (time=0) results were used. Overall, 180 patients were included. The median time from diagnosis to recruitment was 3 weeks. The median age was 51, and 71% of the participants were women. When stratified by CAM use, Chinese patients more commonly used CAM, and oral tablets/powders and acupuncture were the most common forms of CAM. Full details are in Table 1:
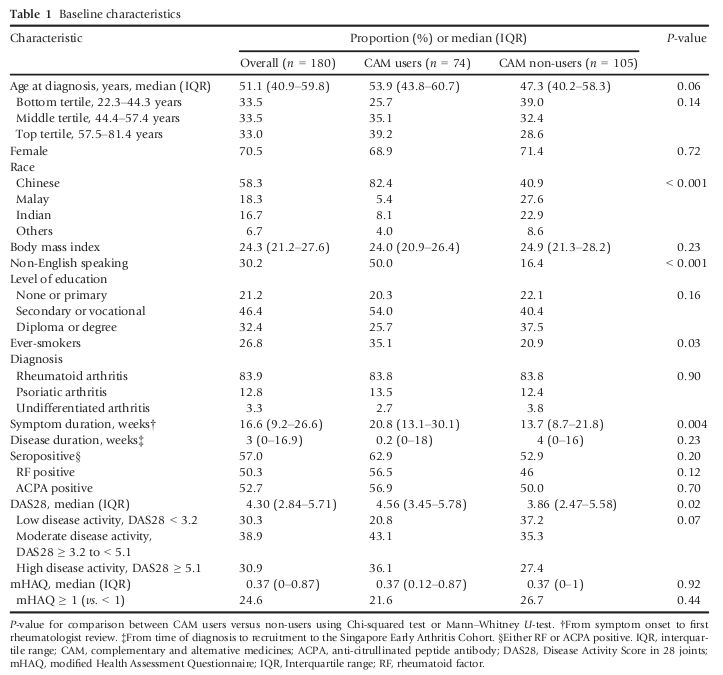
Table 1: Baseline Characteristics
The CAM stratification also shows some additional differences between the groups. There are race, language, and smoking histories that are quite different. Note that the duration of symptoms (until rheumatologist review) was 13.7 weeks among non-users and 20.8 weeks among CAM users. That is, CAM users waited almost twice as long to see a specialist, compared to non-users. Not surprisingly, this meant a delay to the initiation of disease-modifying anti-rheumatic drugs (DMARDs). Figure 1 shows the overall difference between CAM users and non-users: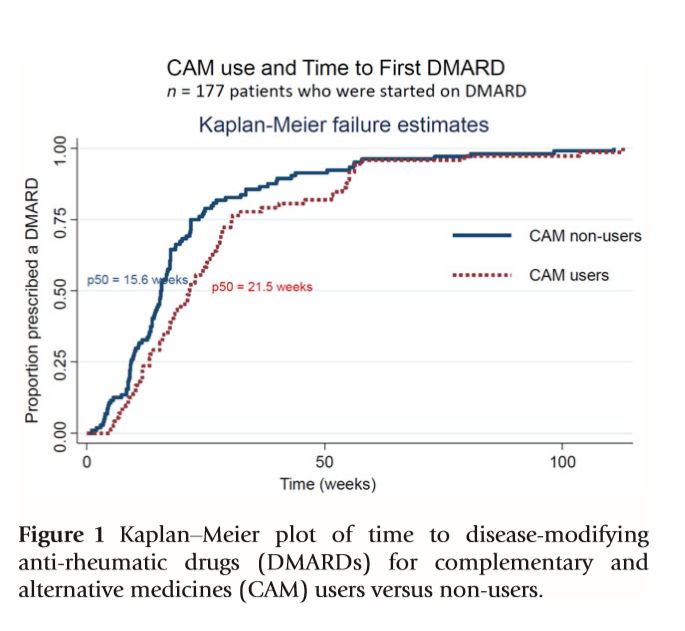
Only CAM use was significantly associated with the time to first DMARD initiation.
CAM use delays effective arthritis therapy
This small study illustrates what appears to be an unfortunate consequence of CAM use: It may be contributing to delays in seeking effective therapies, which may have additional negative consequences. While this study does not show direct harms from CAM use, the relationship between earlier therapy and positive disease outcomes is well established. The authors conclude that patient and public education programs to raise awareness about EIA, and the importance of early treatment, are essential. I would add that continuing to raise awareness of the limitations of CAM, and the consequences of its use, need just as much awareness.